Radiotherapy is one of the mainstay treatments for esophageal cancer. It can be given (1) concurrently with chemotherapy before surgery in resectable cases, (2) concurrently with chemotherapy as definite treatment for unresectable cases, and (3) palliative treatment to relieve obstructive symptoms, pain, or bleeding from tumor.
Radiotherapy uses high-energy beams to destroy cancer cells and it unavoidably irradiates nearby healthy tissues. Proton therapy is a type of radiation therapy that uses beams of high-energy protons to treat cancer. In esophageal cancer, proton therapy can be used to destroy cancer cells and shrink the tumor, either alone or in combination with other treatments such as chemotherapy or surgery.
Compared to traditional photon radiation therapy, proton therapy has some potential advantages when treating esophageal cancer. One advantage is that protons are less likely to damage healthy tissues beyond the tumor leading to fewer side effects. This can be particularly beneficial in esophageal cancer, where the close proximity of the tumor to critical structures such as the heart, lungs, and spinal cord. In addition, higher radiation dose can be given safely to the tumor while minimizing unnecessary dose to the healthy tissues. This can lead to reduced side effects from radiation, potentially improved tumor control, improved quality of life, and lower risk of secondary cancer.
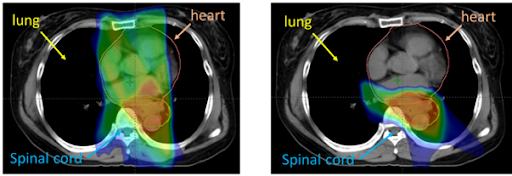
At HPSP, the esophageal cancer patients will be treated with the advanced proton therapy technique using pencil beam scanning, called intensity modulated proton therapy (IMPT). This technique allows a highly conformal dose distribution to the target and highly precise dose delivery thus reduce the risk of radiation exposure to the nearby normal organs. Several studies reported that proton beam therapy generated lower doses to the surrounding healthy tissues, consistent with results from our group (Oonsiri S, Kitpanit S, Kannarunimit D, Chakkabat C, Lertbutsayanukul C, Prayongrat A. Comparison of intensity modulated proton therapy beam configurations for treating thoracic esophageal cancer. Phys Imaging Radiat Oncol. 2022 Apr 28;22:51-56.).
However, it is important to note that proton therapy might not be suitable for every patient, and that the best treatment plan for each patient will depend on several factors, such as the stage and location of the tumor, patient’s overall health, and patient’s personal preferences. A multidisciplinary team of specialists, including medical oncologists, radiation oncologists, and surgeons, can help determine the most appropriate treatment plan for each individual case.

Since 2022, we launched the first multi-center clinical trial in Thailand to compare X-ray (IMRT) versus proton therapy in esophageal cancer treatment <i>(Lertbutsayanukul C, Kitpanit S, Kannarunimit D, Chakkabat C, Oonsiri S, Thephamongkhol K, Puataweepong P, Katanyoo K, Sukhaboon J, Tovanabut C, Chongsathientham S, Treeratsapanich P, Soonthornrak J, Prayongrat A. High-dose Intensity-modulated proton therapy versus Standard-dose Intensity-modulated RadIation therapy for esophageal squamous cell carcinoma (HI-SIRI): study protocol for a randomized controlled clinical trial. Trials. 2022 Oct 22;23(1):897). </i>We expect that the results of this study will establish benefit of proton therapy in esophageal cancer treatment.